Many people have come to believe that the only way to protect Americans against future pandemics is to turn over control of our health care system to the government. The folly of this view was apparent when the U.S. Centers for Disease Control & Prevention (CDC) utterly failed as the monopoly supplier of COVID-19 diagnostic testing kits. When the first cases appeared, about half of the test kits failed and replacements were slow in coming. In addition, the federal response was to issue a state of emergency that literally stopped private labs and universities working on alternative tests in their tracks. At that point, any work on COVID-19 test development required an Emergency Use Authorization from the U.S. Food and Drug Administration (FDA). Valuable time was lost when scientists had to stop what they were doing to apply for permission to develop COVID-19 tests. Also lost was the opportunity to engage in large-scale testing and quarantine hotspots before the coronavirus had spread.
How would a free market health care system respond to a pandemic? For one thing, most Americans would have more options and more control over how their health care dollars are spent. Millions of Americans would likely have more products in their medicine cabinets to assess their health status and provide their physicians with better, faster information. Americans would likely have higher tech versions of many of the items they possess today, like blood pressure cuffs to manage hypertension and pulse oximeters to assess oxygen saturation. They may have more advanced items such as iPhone EKGs and smartphone endoscopes allowing their doctors to examine cardiac health and throats remotely. Patients would also likely have smart thermometers that updated their personal health records automatically in the event of a fever and notified their physicians wirelessly.
Engaged patients may even want a computer app that tracks their health, advises them on developments and contains far more information about their health status than their physicians’ files contain today. Many Americans use programs like Quicken to track their finances. Under a free-market health care system with Large HSAs or MediSave accounts (like in Singapore) consumers may have Quicken Health to manage their medical care. Patients would input health complaints for their doctors to review. The sponsoring software developers would aggregate anonymous data with millions of other Americans, drawing inferences on diseases, conditions, health status and therapies to prevent or better manage chronic conditions.
Under a system where Americans control much of their health care spending, most doctor visits would probably be the result of Quicken Health suggesting patients schedule a consult for a new medical development from a lab result. Physician visits could be on the phone or online similar to a Zoom meeting. Multiple firms would compete on price and convenience to make laboratory and diagnostic testing easily available at rates far below what many pay today. People experiencing a fever would quickly notify their doctors electronically, allowing others to know when and where social distancing was necessary due to flu, colds or worse. It would also allow health authorities to track pandemics or flu season exposure in real time.
Under a free-market health care system, consumers would have more options because providers – hospitals, doctors, clinics and drug makers – would compete for patients’ patronage with patient-pleasing amenities. (This is already done in the cosmetic medical marketplace, by the way).
Why is our health care system so bureaucratic and expensive? There are a variety of reasons, but the government is the biggest culprit. A 70-year old tax law is why millions of Americans have health insurance through their jobs rather than personal and portable health insurance. Rules on medical licensure, scope of practice along with FDA regulations make our health care system more bureaucratic than need be. Virtually all medical care, other than self-care with over-the-counter medications, must begin with an in-person office visit to a licensed physician. Telemedicine has been slow to catch on because third party payers are never on the lookout for new ways of spending their money. By contrast, consumers are always looking for more convenience and better deals.
A critical shortage of personal protection equipment endangered health care workers when the demand far exceeded the supply. Although it isn’t difficult for manufacturers to produce such things as ventilators, masks, gowns and gloves, what is difficult is getting FDA approval to market them. The process takes from months to years in some cases. It wasn’t always that way. Earl Bakken and his brother-in-law, the cofounders of Medtronic, literally developed the first cardiac pacemaker in their garage. It was the late 1950s and their prototype was tested in a hospital and put to use saving lives about a month later. Nowadays all medical equipment must go through a rigorous process of regulatory compliance with design, good manufacturing practices and approval to market prior to being offered to the public. Although quality is important, this raises prices and creates barriers for aspiring entrepreneurs hoping to produce medical supplies and equipment.
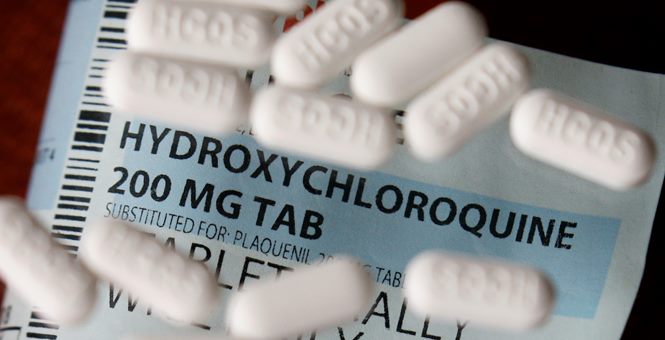
If the health care marketplace were less regulated, patients would also have greater rights to try experimental and novel medicines than they have today. Chloroquine and hydroxychloroquine are both antiviral medications to treat malaria. They are also used to treat autoimmune disorders like rheumatoid arthritis and lupus. There is anecdotal evidence that hydroxychloroquine, azithromycin (an antibiotic) and zinc (a dietary supplement) may reduce COVID-19 symptoms in some patients. Yet, some state medical boards have moved to restrict COVID-19 patients’ access to these drugs because they believe the science does not yet support off-label prescribing.
The U.S. health care system is bureaucratic, costly, inconvenient and decidedly nonpatient-friendly. It doesn’t have to be that way.
This essay is based on a Heritage Foundation report coauthored with John C. Goodman.
0 Comments